Blastic plasmacytoid dendritic cell neoplasm (BPDCN)
Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is a very rare type of cancer. It develops from immature blood cells called plasmacytoid dendritic cells.
Download our booklet about BPDCN
Download our factsheet about BPDCN
Summary
- Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is a very rare type of cancer.
- We do not know exactly what causes it. But it is not because of anything you have or have not done.
- Most people with BPDCN have skin symptoms at first. But your symptoms depend on which parts of your body are affected.
- Doctors usually diagnose BPDCN using skin tests, bone marrow tests and blood tests.
- BPDCN can be difficult to treat. Your doctor will suggest the most suitable option for you based on your individual circumstances. This might be:
- Chemotherapy
- Treatment as part of a clinical trial, if there is one suitable for you
- Tagraxofusp, a medicine designed to target BPDCN cells, if you are able to access it
- A treatment usually used for other blood cancers
- A stem cell transplant, if you are fit enough to have one
- Medicines to prevent or treat symptoms or side effects
- We are here for you if you need support.
Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is a type of cancer.
 It develops from an immature type of blood cell called a plasmacytoid dendritic cell. If you have BPDCN, these cells grow out of control and can build up in your:
It develops from an immature type of blood cell called a plasmacytoid dendritic cell. If you have BPDCN, these cells grow out of control and can build up in your:
- Skin
- Bone marrow: the spongy centre of some of your larger bones where blood cells are made
- Lymph nodes: small, bean-shaped structures throughout your body that are part of your immune system
- Spleen: a fist-sized organ under your ribs on the left side that filters and stores blood and makes some blood cells
- Other parts of your body
BPDCN is very rare. Only 20 to 30 people are diagnosed with it in the UK each year.
- BPDCN typically affects people over 60, but it can develop at any age, even in children.
- It is much more common in men than in women, but we don’t know why this is.
- It can affect people of any ethnic background.
We do not know exactly what causes BPDCN. But it is not because of anything you have or have not done.
You cannot catch BPDCN or pass it on to anyone else.
BPDCN is not inherited. You did not get it from your parents, and you cannot pass it on to any children you may have.
Symptoms of BPDCN vary from person to person. They can be quite vague at first, which makes BPDCN difficult to diagnose.
Most people with BPDCN have skin symptoms. These might be:
- Bruise-like patches
- Small lumps
- Larger lumps
- Raised scaly patches
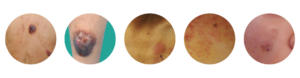
You might only have skin symptoms in one or two places, or you might have lots of them all over your body. You might also have patches inside your mouth.
Without treatment, BPDCN usually progresses to involve your bone marrow and other parts of your body. If this happens, you might have symptoms like:
- Feeling tired, breathless or dizzy
- Infections that last a long time or keep coming back
- Bruising easily or bleeding when you wouldn’t usually (for example, nose bleeds or bleeding gums when you brush your teeth)
- Tummy pain, bloating or feeling full very quickly when you eat
- Swollen lymph nodes
- Headaches, confusion, fits (seizures) or vision changes
You might get other symptoms, depending on which parts of your body are affected.
BPDCN can be difficult to diagnose because the symptoms are often vague. You will probably see a skin specialist first. If they think you might have BPDCN, they will refer you to a blood specialist.
They usually diagnose BPDCN using:
- Skin tests
- Bone marrow tests
- Blood tests
- Other tests
Your medical team might take a while to rule out other conditions before testing you for something as rare as BPDCN. This means getting a diagnosis can take time.
It can be difficult waiting for tests and test results. Our Helpline on freephone 08088 010 444 is here for you if you need support.
Skin tests
Your dermatologist might measure any patches or lumps you have on your skin, and take photos of them. They will also numb an affected area of your skin and take a small sample of it. This is called a skin biopsy.
They send the sample to the lab for testing.
Bone marrow tests
If your team think you might have BPDCN, they usually do a bone marrow test. Bone marrow is the spongy part in the middle of some of the large bones in your body. It is where your blood cells develop.
To have a bone marrow test:
- You have an injection to numb the area first.
- Then a doctor uses a specialised needle to take samples of your bone marrow, usually from your hip bone.
- They send the sample to the lab for testing.
Blood tests
You will have blood tests to:
- Measure your numbers of red blood cells, white blood cells and platelets
- Check how well your liver and kidneys are working
- Check how well your blood clots
Your blood samples will also go to the lab for specialised tests.
Other tests
You might have other tests to find out more about how BPDCN is affecting your body. These are not always needed, but they could include:
- A test to take a sample of a lymph node (a lymph node biopsy), if they are swollen
- A test to take a sample of the fluid around your brain and spinal cord (a lumbar puncture) to check for BPDCN cells
- Scans to check for BPDCN in your lymph nodes, spleen or liver
- Other tests recommended by your medical team
Lab tests
Your samples go to the lab for specialised tests. Scientists will look for BPDCN cells under a microscope. They will also test the samples to find out what proteins are on the surface of your cells, and to look for any genetic changes in your cells. These tests help them make an accurate diagnosis.
There is no standard approach to treatment for BPDCN and different doctors might use different options. Your medical team will suggest the most suitable treatment for you based on:
- Your symptoms and test results
- Your age and overall fitness
- Your personal preference
- Any other medical conditions you have
- Whether you’ve had treatment for BPDCN before
- Any side effects you may have had with other treatments
There are a number of treatment options they might consider. Many of these are quite intensive, because BPDCN is fast-growing. This means it needs aggressive treatment even if you only have a few skin problems to begin with.
Chemotherapy
The first treatment for BPDCN is usually chemotherapy.
Different chemotherapy medicines may be used to treat BPDCN. These are usually based on treatments that have been successful in other cancers affecting the blood or bone marrow, like:
These treatments are quite intensive, and they are only suitable for people who are fit enough to have them. If you are older, or have other medical conditions, your team might suggest gentler chemotherapy medicines.
Your medical team will tell you exactly what chemotherapy medicines they recommend for you. They will explain what the treatment is, how you have it, and what side effects you might get.
Macmillan have more information about particular chemotherapy combinations.
Alongside your standard chemotherapy, you may also need to have chemotherapy medicines injected into the fluid surrounding your brain and spinal cord. Your doctor will do this through a needle in your back. This treats BPDCN in your central nervous system, and also reduces the risk of BPDCN coming back.
Treatment as part of a clinical trial
Your medical team might suggest treatment as part of a clinical trial, if there is one suitable for you. This could let you access treatments that would not be available otherwise.
If there is a clinical trial that might be suitable, your medical team should explain what it would involve, and the risks and benefits of taking part. They will give you the information you need to decide if it’s something you’d like to do. It is your choice whether or not to take part.
Stem cell transplant
If you respond well to your initial treatment for BPDCN, your medical team might recommend a stem cell transplant. This aims to reduce the risk of your BPDCN coming back. In some people, it may lead to a long-term remission.
A stem cell transplant is very intensive. It is only suitable for people who are fit enough to have it.
Your medical team should let you know if a stem cell transplant is an option for you. They will discuss it with you and give you a chance to ask questions.
We have separate information on stem cell transplants.
Targeted treatments
Targeted treatments are drugs designed to block specific proteins on cancer cells. This means they kill cancer cells with as few effects on healthy cells as possible.
At the time of writing, tagraxofusp is the only targeted treatment that has been developed to treat BPDCN. But some targeted treatments used in other blood and bone marrow cancers may also be an option.
Tagraxofusp
Tagraxofusp is approved to treat BPDCN in the US and Europe. At the time of writing, it is not approved in the UK. Children may be able to access it through a compassionate access scheme. There is not currently a similar scheme for adults. Your medical team may be able to tell you if there is any way to access it. But it may not be possible in the UK.
Tagraxofusp is a targeted medicine that was specifically developed to treat BPDCN. Its brand name is Elzonris.
The European Medicines Agency have more information about tagraxofusp. Or you can read more about it in our downloadable booklet on BPDCN (PDF).
Targeted treatments used for other cancers
Some targeted treatments used to treat other blood or bone marrow cancers might be helpful for people with BPDCN, but there is not much evidence to support their use. Your medical team might suggest one of these treatments, especially if chemotherapy is not suitable for you, or if BPDCN has come back after chemotherapy.
Medicines your team might suggest include:
These medicines are not approved to treat BPDCN, but your medical team might use them off-label. This is when a doctor prescribes a medicine that’s approved for one condition to treat a different condition.
Your medical team might suggest a different targeted treatment for you. They will explain why they think it might be suitable and give you information about it.
Some of these treatments might be funded by your hospital, but some might not. If you’re in a position to, you may be able to pay to access them through your hospital. Or you may be able to have some treatments that are funded combined with some that you pay for.
Macmillan have more information about particular cancer treatments. You can search for your treatment or choose the ‘Treatment and drugs A to Z’.
Supportive care
You might also need medicine to prevent or treat symptoms or side effects. This is called supportive care. It does not treat your BPDCN itself, but it helps you feel better. It aims to reduce your symptoms, extend your survival, and give you and your loved ones the best quality of life possible.
Supportive care might include:
- Blood transfusions or medicines called growth factors, if your blood counts are too low
- Anti-sickness or anti-diarrhoeal medications
- Pain relief, if you need it
- Medicine to prevent or treat infections
- Mouth washes to help with mouth ulcers, oral thrush or a sore mouth
- Food or drink supplements, if you are not able to eat or drink enough
- Steroids, which reduce inflammation in your body and can help with many different symptoms
Supportive care can also include:
- Psychological support
- Support with exercise or physiotherapy
- Social support
- Spiritual wellbeing such as mindfulness
Your medical team should talk to you to find out what support they can offer you. Let them know if you have any symptoms or side effects that you are finding hard to cope with.
BPDCN is an aggressive type of cancer. It can be difficult to treat, and it often comes back.
As with most cancers, outcomes vary from person-to-person. They depend on lots of different factors, including:
- Your age and overall fitness
- Whether BPDCN is in your skin or in other places too
- Any other blood or bone marrow conditions you have
- How well you respond to your first treatment
Your medical team are best placed to discuss what they expect for you because they know your individual circumstances.
If your BPDCN does not respond to treatment, or comes back after treatment, your medical team will talk to you about your options. These depend on what treatment you’ve already had and how you responded to it. Your medical team might suggest:
- Treatment as part of a clinical trial, if there is one suitable for you
- A treatment you have not had before, followed by a stem cell transplant if you are fit enough and it is a suitable option for you
If there are no suitable treatment options left, they might suggest end of life care.
End of life care means you do not have any more treatment that aims to control or cure your BPDCN. But you still have treatment to relieve your symptoms and improve your quality of life. End of life care begins when you need it and may last a few days, months or years.
End of life care helps you live as well as possible until you die. The aim is to help you have a good quality of life and die with dignity.
We are here for you if you need support with end of life care. Call our freephone helpline on 08088 010 444, message us on WhatsApp at 07500 068065 or email us at support@leukaemiacare.org.uk.
The following charities also provide support and information for people dealing with end of life care:
It can be helpful to hear about people who’ve been in a similar situation to you. Here, Becki Lucas shares her experience of BPDCN, including practical tips that helped her cope.
Downloads or relevant links
We have more information on:
We also have a booklet about BPDCN that you can download. Or, if you’d prefer a short summary, we have a two-page factsheet.
Need support?
We are dedicated to ensuring that anyone affected by leukaemia receives the best possible diagnosis, information, advice, treatment and support.
If you need support with any aspect of your or a loved one’s diagnosis:
- Call our free helpline on 08088 010 444 or send a WhatsApp message to 07500 068 065 (services available Monday to Friday, 9am to 5pm).
- Visit our support page to find out about our other services, including support groups, one-to-one buddy support, financial support or counselling
Help us improve our information
We aim to provide information that’s reliable, up-to-date, and covers what matters to you. We want you to feel supported and able to be involved in decisions about your care. Please complete our short survey to help us improve our information and make sure it meets your needs.
If you’d like a list of the references we used to develop this information, please email information@leukaemiacare.org.uk
Review date
Last updated: June 2024
Review date: June 2027

 chat
chat

